An overview of findings and recommendations regarding healthcare for people with disability
The highly anticipated Final Report of the Independent Review of the National Disability Insurance Scheme (NIDS) was released on 7th December 2023.
The wide-ranging review began in October 2022, with a goal to “look at ways to improve both the experience of participants in the scheme and their outcomes.” The review panel was also asked to identify “ways to make sure the scheme is sustainable so it is around for years to come.”
Consultation for the review was extensive. It included hearing from 10,000 people, receiving 4000 submissions and collecting more than 2000 hours of “deeply personal stories from people with disability.”
The Final Report makes 26 recommendations, each including a series of detailed actions (139 in total).
At SeenCare, our mission is to change how care is delivered for NDIS participants with high medical needs. Therefore, in this article, we’ll provide an overview of the main findings and recommendations from the NDIS Review that relate to healthcare for people with disability.
Some important context
Before going any further, it’s important to note that the NDIS Review is about more than the NDIS.
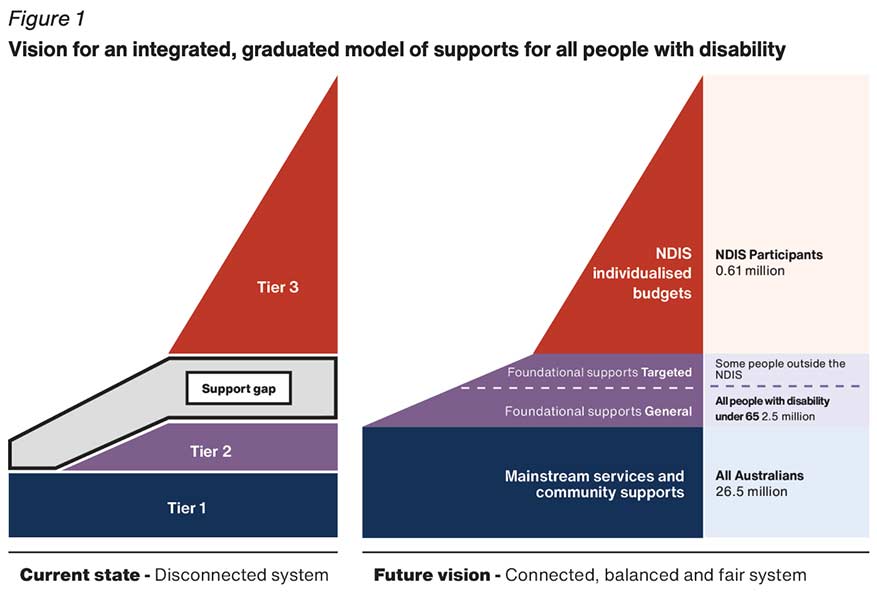
Many of the recommendations cover government-funded services as a whole, such as education, health and justice (referred to as ‘mainstream services’). Plus, the Final Report also discusses non-NDIS services for people with disability, which it calls ‘foundational supports.’
We won’t get into foundational supports in this article, other than to highlight they are proposed as a way to fill a ‘support gap’ that currently exists between mainstream services and individuals with NDIS funding (the purple component in the image below).
Figure 1, p.35 of the Final Report
Beyond the NDIS
Explaining the rationale for expanding its scope outside the NDIS, the Review Panel states:
“Our view is that you can’t fix the NDIS without fixing everything around it. For this reason our recommendations go beyond the NDIS. We want to create a new system of support, including accessible and inclusive mainstream services, a new system of foundational supports as well as the NDIS. This will make sure the 2.5 million Australians with disability under 65 can get what they need.”
Now that we’ve got the high level context out of the way, let’s go a little deeper to pull out some of the points from the review that could have an impact on providers (and participants).
Implications for health and disability services
Below are 5 key insights from the Final Report on the NDIS Review that will shape the healthcare and disability landscape in the coming years.
1. A spotlight on equity (and rights)
The NDIS Review comes on the back of the 2019 Royal Commission into Violence, Abuse, Neglect and Exploitation of People with Disability.
The Final Report explains, “While our Review and the Disability Royal Commission were different in scope and focus, there have been many common observations and recommendations.”
When it comes to the experience of people with disability with healthcare, many of these commonalities stem from:
- Barriers to accessing healthcare
- Experiences of exclusion from healthcare
- Receiving a substandard quality of care
Discussing this challenge, the Commission states, “Too often, people with disability have received poor care, the wrong care or no care.”
Their recommendation is to “change the structure of the system to support – not discourage – integrated care.”
Integrated healthcare and disability services (like the model we use at SeenCare) are now firmly seen as a human right for people with disability—not a ‘nice to have.’
2. Addressing “the oasis in the desert”
This eloquent phrase sums up what many of us working in public healthcare and community support services have experienced since the rollout of the NDIS, yet struggled to put into words.
The Final Report states (p.25),
“In trying to correct for the underfunded, inconsistent and unfair arrangements that existed prior to the NDIS, governments have come to rely on the NDIS as the dominant, and in some cases only, source of supports for people with disability — the oasis in the desert.”
This cuts both ways in healthcare and disability services.
On the medical side, clinicians will be familiar with countless examples of huge discrepancies between patients who are able to access NDIS funding (the oasis), and those stuck in the desert trying to make do with the sparse community supports available outside of the NDIS.
For disability service providers, most practitioners have witnessed the difference in outcomes for those with an engaged medical practitioner, compared with those constantly running into the barriers to accessing quality medical care discussed in the previous point.
As we’ll see in point three, the Review Panel is adamant that this ‘oasis and the desert’ dynamic must come to an end.
3. Rethinking boundaries
Discussing the often difficult to navigate boundary between healthcare and disability services, the Final Report for the NDIS Review claims, “The framework which governs the relationship between the NDIS and other service systems – the Applied Principles and Tables of Support (APTOS) – has failed.”
They go on to explain, “It is based on the idea that there is a hard line between the NDIS and other systems. Despite its intent, it has led to seemingly endless arguments about who does what and who pays for it.”
Now. If you’ve never heard of the APTOS, don’t worry. You don’t need to be familiar with the framework to understand the intent of the above statements.
In short, the Review Panel gave a clear recommendation that a new way of determining boundaries between NDIS and health services is required.
How this will work is anyone’s guess. But, as a health or disability services provider, it could be worth considering how your organisation might effectively collaborate with partners from ‘the other side.’
For example, as SeenCare, we formed a partnership with a small group of GPs with an interest in disability, who agreed to provide bulk billed GP support to all SeenCare NDIS clients.
4. Coordination is key
Coordination between systems (or the lack of it) is a consistent theme throughout the NDIS Review.
The Final Report explains, “The introduction of the NDIS and its often complex interface with many mainstream services has made navigating multiple systems more difficult.”
Again, one of the contributing factors to this challenge is the impractical framework for boundaries between services, where it is assumed “people with disability will be supported by the NDIS or another system.” However, when it comes to healthcare and disability services, we would argue that a lack of shared objectives also plays a role.
In many instances, a lack of coordination stems from two services working on overlapping, yet somewhat conflicting goals.
For example, the team at a diabetes clinic might be working on gaining the tightest control possible of a participant’s blood sugar levels. At the same time, the disability support provider could be implementing measures to increase freedom and autonomy, in line with the overarching goals in the participant’s NDIS plan.
In this situation, effective interagency coordination would require both services to come together with the participant to decide on a unified way forward
5. NDIS and hospitals
It’s long been recognised that communication and collaboration between the NDIS and hospitals has room for improvement.
In a section titled, ‘Interaction between NDIS and hospitals,’ (p.69) the Final Report discusses challenges around discharge planning.
The key issues identified are:
- Significant delays in discharge for people with disability
- A lack of clear discharge and transition plans
- Poor communication and information sharing between the NDIS and health systems
- Inconsistent and drawn out NDIA planning processes
The review states that these issues remain, “Despite recent efforts driven by Disability Reform Ministers and the NDIA, including the introduction of Hospital Liaison Officers.”
The review will likely result in further new initiatives to improve collaboration and coordination between hospitals and the NDIS.
In the meantime, to do our bit in addressing this challenge, we’ve utilised our combined 54 years of experience in the disability and healthcare sectors to create a Post Hospital Care Service. This service has the capacity to provide high-level support to NDIS participants being discharged from hospital.
Toward a unified system
The common thread throughout the Final Report for the NDIS Review is the importance of moving toward a more “connected, balanced and fair system.”
Dozens of recommendations and detailed actions outline a blueprint for how this can be achieved. But a simple yet powerful statement in the guide for people with disability and their families sums up the pathway best:
We are recommending that all governments work together to plan and fund a new system of support. The NDIS is one part of this system. But it must also include more support for people with disability who are not eligible for the NDIS, through foundational supports.
For healthcare and disability services providers, it may be business as usual for some time still.
However, for those wishing to build the innovative services that are likely to become the cornerstone of the new system of support, the Final Report of the NDIS Review provides a wealth of information that can be used to transform how care is delivered.
If you would like to find out more about SeenCare’s unique model of integrated health and disability care, please contact one of our friendly staff members today.